Cynthia Campos-Moreno ¹ , Manuel González-Díez ¹ , Clara Isabel Murillo-Hermosilla ¹ , Cristina Perea-García ¹ , Amanda Sánchez-Arés ¹
1 Estudiante del Máster en Neurociencias Básicas Aplicadas y Dolor de la Universidad de Granada (UGR)
TRANSLATED BY:
Beatriz Pérez-Cortés ² , Amy McCullough ² , Beatriz Moreno-Cuadrado ² , Lourdes Ureña-Pérez ² , Marta Giménez-Polo ² , Ígor Iribar-Revuelta ²
2 Student of the BA in Translation and Interpreting at the University of Granada (UGR)
This review aims to gather the most relevant data regarding mindfulness and its effectiveness towards chronic pain treatment. In order to do so, we carried out a bibliographical study on the areas of the brain which are activated by chronic pain and the influence of mindfulness on these areas. In addition to this, we studied the effectiveness of mindfulness by itself and, in comparison with other non-pharmacological therapies, its effects on patients depending on their age. Despite the apparent contradictions in its action mechanisms, mindfulness seems to be as effective as other non-pharmacological therapies when used as an adjuvant therapy, regardless of the age group. Thus, it could be useful for preventing abuse or reducing dependence on analgesics.
Keywords: chronic pain, mindfulness, neuroimaging, pain management, alternative therapies, pediatric pain, geriatric pain.
Introduction
Chronic pain is often defined as any pain lasting longer than 3 months, or any pain persisting after the normal time for tissue healing (1). It can worsen progressively and appear intermittently, thus decreasing the patient’s quality of life. It is estimated 5.5%-33% of the global adult population suffer from chronic pain. Furthermore, adolescents and children can also suffer from chronic pain. The number of people affected has increased over the years due to the population aging (2). This leads to economic costs for both the healthcare system and the professional careers of the patients, as it can result in a loss of productivity (1) or even in workplace absenteeism (3), consequently affecting the employer.
Over the last two decades, one of the most common treatments used for chronic pain has been opioid prescriptions (4), since they are effective analgesics. Nevertheless, due to an exponential growth in the prescription of these drugs, the death rate by overdose has increased (2), as well as the addiction likelihood. Thus, researchers are exploring the use of combined treatments (pharmacological and non-pharmacological) in order to reduce the use of opioids (4). Among the non-pharmacological treatments, certain alternative therapies can be found. Most of these have been proved to be effective in treating chronic pain and are cheaper, thus reducing economical costs. These alternative therapies include mindfulness-based interventions, the cognitive-behavioral therapy (CBT), the acceptance and commitment therapy, acupuncture, and hypnosis (4). All of these treatments are able to reduce pain perception and improve the functionality of the patient. In addition, other types of therapy, such as occupational therapy, physical therapy, and physical exercise, have been effective in chronic pain treatment (2). In this paper, we focus on mindfulness-based interventions.
Mindfulness-based interventions (e.g. yoga, meditation, stress reduction) are based on the non-judgmental awareness of the present moment (2), by focusing on it and accepting it (1). This allows patients to cope better when they experience pain (3). Accordingly, the aim of this practice is to reduce pain perception and improve the patient’s quality of life. Although it is often impossible to eradicate chronic pain, patients can learn skills to help them live a productive life, even when experiencing a feeling of discomfort (2).
The role of mindfulness is promising, but there are certain limitations because only a small number of studies have been carried out in this line. These limitations include the variability of the population and the different techniques that can be used (3) as well as the low quality of these studies (5), making their standardization and generalization more difficult.
Despite these limitations, some advantages have been found, including the improvement of symptoms; the lack of abuse or dependence; and the improvement of comorbid conditions, such as anxiety or depression (2, 3). In this review, we aim to show alternative treatments which carry no risk of addiction for patients who are suffering from chronic pain. The main focus is set on mindfulness and its actual effectiveness as a treatment.
- Neurophysiology and neuroimaging
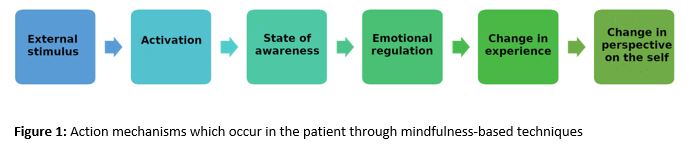
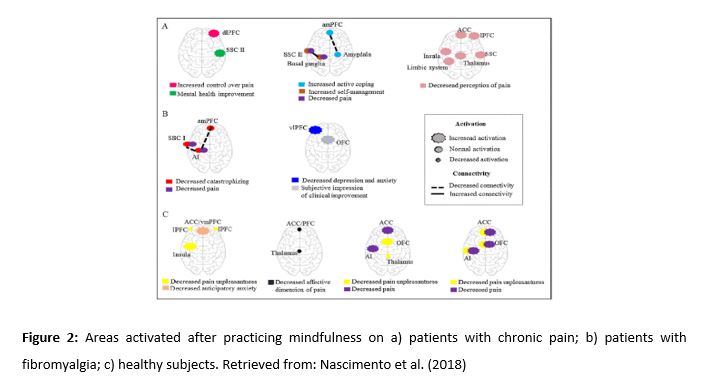
The applications of mindfulness are well established. However, its action mechanisms are still unclear (Figure 1). In order to explain how these therapies work, four interrelated components were proposed (Figure 3): attention regulation, body awareness, emotion regulation, and change in perspective on the self (6). The first three components will be thoroughly explored. Afterwards, the elements that constitute pain, how they are represented in the brain, and how mindfulness affects the areas in which they are involved in will also be studied.
The action components of mindfulness and pain are explained as follows:
2.1. Attention regulation
Attention regulation is defined as the process of focusing attention on an object, recognizing distractions and going back to focusing on the object. Many studies (7, 8) suggest a greater activation of the anterior cingulate cortex (ACC) and the secondary somatosensory cortex (SII). Both areas are involved in the process of attention regulation.
2.2. Body awareness
Body awareness refers to the process of focusing on a structure or task inside the body. There are two possible mechanisms involved in the increase of body awareness. The first one would involve the activation of the right anterior insula and the long-term concentration of gray matter within this area. The other possible mechanism would involve the regulation of the amygdala via the ACC and the dorsolateral prefrontal cortex (dlPFC). However, short-term studies suggest that these changes start at the temporoparietal junction, and not at the insula (6, 9).
2.3. Emotion regulation
Emotion regulation occurs at a cognitive level (focused attention). It is based on playing close attention to stimuli and to changes, and how we respond to them. This can be achieved either by the reappraisal of the stimulus (i.e. interpreting the stimulus in a positive way) or by the extinction of the stimulus (i.e. reverting the response to the stimulus). Another way in which emotion regulation occurs at a behavioral level is by inhibiting the expression of certain behaviors in response to the stimulus (6).
Two systems have been suggested: (1) a system that involves the lateral prefrontal cortex (lPFC) and the ventral prefrontal cortex (vPFC) and whose functions are, respectively, managing selective attention and participating in the inhibition of a response; and (2) a system that involves the ACC (6, 10).
2.4. Pain
According to Bilevicius et al. (11), pain is composed of three factors: (1) a sensorial factor, which activates the primary and secondary somatosensory cortices (SI and SII) and the thalamus; (2) a cognitive factor, which activates the prefrontal cortex (PFC); and (3) a motivational-affective factor, which increases the activity in the ACC and in the anterior and posterior insulae. Mindfulness acts directly or indirectly in many of these factors, as previously seen.
2.5. Neuroimaging results
A study carried out by Grant et al. (12) revealed that experienced meditators show a greater activation of the insula, the thalamus and the midcingulate cortex, as well as a minor activation of the areas of the brain that are responsible for emotion control (the medial prefrontal cortex [mPFC], the orbitofrontal cortex [OFC], and the amygdala). This would allow meditators to pay more attention to the sensory input of stimuli and to inhibit any emotional appraisal or reactivity. This situation, according to the researchers, leads to a diminished sensitivity to pain.
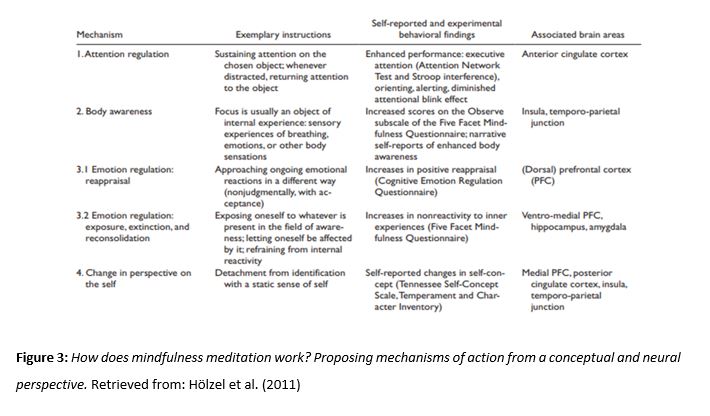
On the other hand, Nascimento et al. (13) reported an increase in the activation of the dlPFC, the ventromedial prefrontal cortex (vmPFC), the OFC, the SI and SII, and the limbic system in patients suffering from chronic pain (Figure 2). The increase of activity in the dlPFC in the patients occurs when action mechanisms are modified by acute pain. Therefore, this leads to an increase in activity in areas involved in emotion regulation (11).
After having learnt about mindfulness, patients suffering from chronic pain experienced improvements in clinical measures of pain and self-efficacy to deal with chronic pain. Patients also experienced a decrease in levels of anticipatory anxiety, pain intensity and the negative experience of pain (13). These findings suggest that the use of mindfulness decreases the likelihood of presenting psychiatric comorbidities and increases the patient’s capabilities of acceptance and pain control (14). These changes in the experience of pain are mainly associated with a decrease in amygdala activity and an increase in PFC activity (15).
- Mindfulness compared with other treatments
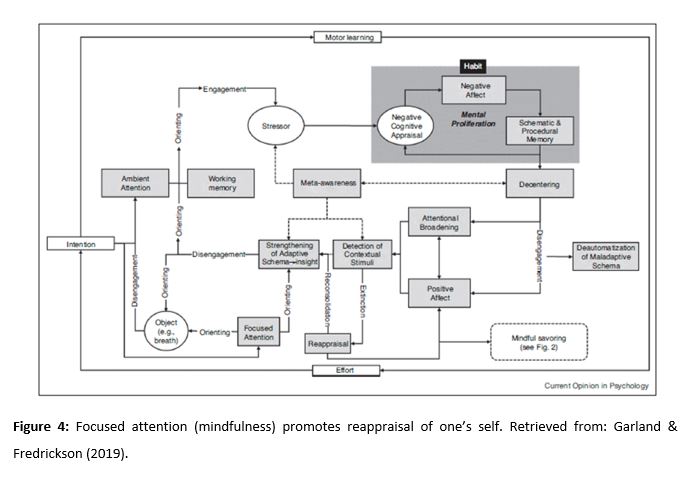
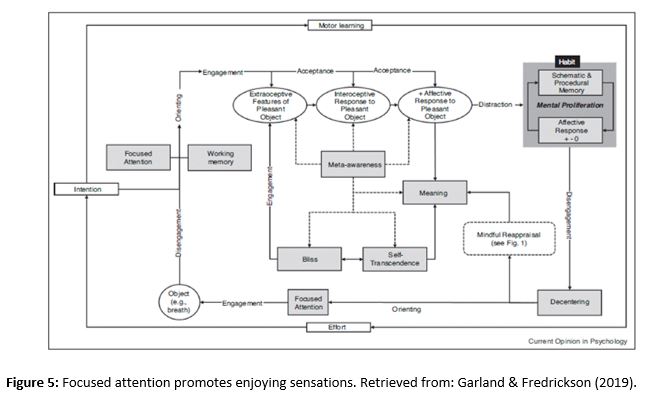
The mindfulness-to-meaning theory (MMT) is based on two premises: (1) the principle that focused attention (mindfulness) promotes reappraisal of one’s self (Figure 4); and (2) the principle that focused attention encourages the individual to enjoy the sensations caused by stimuli (Figure 5) (16).
Recently, certain studies have shown that a period of 8 weeks of mindfulness-based stress reduction (MBSR) increases the efficacy of reappraisal to a similar degree as cognitive-behavioral therapy (17).
Taking these advances into account, Mindfulness-Oriented Recovery Enhancement (MORE) has been created as a treatment for those patients who misuse opioids in order to treat their chronic pain (18, 19). MORE aims at increasing cognitive control, facilitating reappraisal and enjoying pleasant sensations. It also aims at returning the patients’ reward processing back to baseline levels, so that they value natural rewards more than drug-based rewards (20). MORE has been found to significantly decrease chronic pain and drug-seeking behavior (18, 19). In addition, this treatment has also been found to significantly increase MMT mechanisms. These positive effects are linked to a decrease in chronic pain intensity and to a lower risk of drug consumption (18).
Moreover, a systematic review of randomized controlled trials was carried out, aimed at confirming the efficacy of mindfulness-based stress reduction (MBSR) compared to that of cognitive-behavioral therapy (CBT) on patients with symptoms caused by chronic pain (21). A study compared CBT and MBSR and did not find any significant differences between them in relation to the improvement of physical functioning or the reduction of pain intensity (21). The CBT group, however, showed more signs of improvement on depressive symptoms after the treatment compared to the MBSR group. When compared to the control group, both CBT and MBSR were associated with general improvements after the intervention (22).
These results are consistent with those found in a meta-analysis carried out in 2016 and focused on interventions for chronic pain based on acceptance and mindfulness, which showed minor effects on the reduction of pain intensity and depressive symptoms compared to the control groups (5).
3.1. Comparison between different age groups
Mindfulness, like any other treatment, must be adapted according to the characteristics of the patient. The age of the participants has to be taken into account, since children do not have the same comprehension and understanding as adults do. Working with children requires a simpler language, whilst adults are capable of more abstract thinking. A series of studies on different groups are described below and are divided as follows: pediatric population, adult population and geriatric population.
3.1.1. Pediatric population
Several studies confirm that including non-pharmacological therapies in treatments that require drugs can have much more effective results on pediatric population (4). This is due to the fact that a multidisciplinary approach including coping strategies not only improves children quality of life, but also significantly reduces the possibility of dependence and prevents developing a future tolerance. Immediate and sufficient analgesia are necessary to manage acute pain (such as post-operative pain). However, including psychological education of the patient pre- and post-surgery can help manage the pain and speed up the recovery process.
On the other hand, chronic pain management requires a more prolonged analgesia and is more complex to treat, since the patient can feel that pharmacological treatment is insufficient, thus resorting to non-pharmacological methods (23). In a randomized pilot study of an intervention based on mindfulness for adolescent women suffering from chronic pain, the patients reported an improvement in pain management and a decrease in salivary cortisol levels during the post-treatment session (24). However, the quality of this line of research has varied from randomized controlled trials to pilot studies and is very limited due to a small sample size.
3.1.2. Adult population
Regarding adult population, there are studies which have focused on medical conditions such as fibromyalgia, e.g. a study which was carried out on a total of 70 women who met the criteria of the illness (25). In comparison with the control group, the results showed a reduction of IL-10 and higher baseline levels of CXCL8 (immune biomarkers), as well as a change in schemes and a significant reduction of chronic pain. It appears that training in schema modification and relaxation techniques (such as mindfulness) has been able to positively influence clinical symptomatology, as patients reported a decrease in pain, an improvement in psychological inflexibility, and a better quality of sleep.
3.1.3. Geriatric population
Finally, geriatric population includes participants aged over 65. A review of a series of studies which followed mindfulness-based programs analyzed variables such as insomnia and executive function, among others (26). However, the focus is set on chronic back pain (27). The results showed not only an improvement in pain management, but also significantly lower post-treatment pain levels. In addition, the acceptance of chronic pain was higher than in the group that did not receive the mindfulness-based treatment. A 3-month follow-up session showed that the experimental group maintained significantly better results than the control group.
- Conclusions
The way in which the associated areas of the brain allow mindfulness-based therapies to improve symptomatology is still unclear. Some authors have suggested that the main associated areas (i.e. the ACC, the insula, and several sections of the PFC) may play a key role because they are involved in pain and attention processing. They argue that the mixed results are due to a learning process which would make the response of these areas more efficient, thus causing more experienced users to experience activation at a faster rate (7, 8).
Regarding the implementation of mindfulness-based therapies as treatment, they have been shown to be at least as efficient as cognitive-behavioral therapy, with regard to comorbid symptoms of chronic pain. However, there is limited evidence of mindfulness-based therapies influencing pain itself, as it requires traditional pharmacological treatments to reach maximum efficacy (17-20). These effects are constant regardless of the age group, but they must be adapted to the characteristics of each group (21, 22, 24, 27). Due to these characteristics, these therapies could be particularly useful to prevent or reduce the abuse and dependence on analgesics. Future work in this line of research is suggested (2-4, 23).
Conflicts of interest statement
The authors declare that there are no conflicts of interest in this article.
References
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. 2017; 51(2): 199-213. Doi: 10.1007/s12160-016-9844-2.
- Majeed MH, Ali AA, Sudak DM. Mindfulness-based interventions for chronic pain: evidence and applications. Asian J Psychiatr. 2018; 32: 79-83. Doi: 10.1016/j.ajp.2017.11.025.
- Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, Rogozinska E. Does mindfulness meditation improve chronic pain? A systematic review. Curr Opin Obstet Gynecol. 2017; 29(6): 359-366. Doi: 10.1097/GCO.0000000000000417.
- Wren AA, Ross AC, D’Souza G, Almgren C, Feinstein A, Marshall A, Golianu B. Multidisciplinary pain management for pediatric patients with acute and chronic pain: a foundational treatment approach when prescribing opioids. Children. 2019; 6(2): 33. Doi:10.3390/children6020033.
- Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance -and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016; 45(1): 5-31. Doi: 10.1080/16506073.2015.1098724.
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011; 6(6): 537–559. Doi: 10.1177/1745691611419671.
- Hölzel BK, Ott U, Hempel H, Hackl A, Wolf K, Stark R, Vaitl D. Differential engagement of anterior cingulate cortex and adjacent medial frontal cortex in adept meditators and non-meditators. Neurosci Lett. 2007; 421(1): 16–21. Doi: 10.1016/j.neulet.2007.04.074.
- Brown CA, Jones AK. Meditation experience predicts less negative appraisal of pain: electrophysiological evidence for the involvement of anticipatory neural responses. Pain. 2010; 150(3): 428–438. Doi: 10.1016/j.pain.2010.04.017.
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006; 62(3): 373–386. Doi: 10.1002/jclp.20237.
- Zeidan F, Grant JA, Brown CA, McHaffie JG, Coghill RC. Mindfulness meditation-related pain relief: Evidence for unique brain mechanisms in the regulation of pain. Neurosci Lett. 2012; 520(2): 165–173. Doi: 10.1016/j.neulet.2012.03.082.
- Bilevicius E, Kolesar TA, Kornelsen J. Altered neural activity associated with mindfulness during nociception: a systematic review of functional MRI. Brain Sci. 2016; 6(2): 14. Doi: 10.3390/brainsci6020014.
- Grant JA, Zeidan F. Employing pain and mindfulness to understand consciousness: a symbiotic relationship. Curr Opin Psychol. 2019; 28: 192–197. Doi: 10.1016/j.copsyc.2018.12.025.
- Nascimento SS, Oliveira LR, DeSantana, JM. Correlations between brain changes and pain management after cognitive and meditative therapies: a systematic review of neuroimaging studies. Complement Ther Med. 2018; 39: 137-145. Doi: 10.1016/j.ctim.2018.06.006.
- Greeson JM, Chin GR. Mindfulness and physical disease: a concise review. Curr Opin Psychol. 2019; 28: 204-210. Doi: 10.1016/j.copsyc.2018.12.014.
- Reive C. The biological measurements of Mindfulness-Based Stress Reduction: a systematic review. EXPLORE. 2019. Doi: 10.1016/j.explore.2019.01.001. In press
- Garland EL, Fredrickson BL. Positive psychological states in the arc from mindfulness to self-transcendence: extensions of the Mindfulness-to-Meaning Theory and applications to addiction and chronic pain treatment. Curr Opin Psychol. 2019; 28: 184-191. Doi: 10.1016/j.copsyc.2019.01.004.
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: a randomized controlled trial. J Consult Clin Psychol. 2016, 84(5): 427-437. Doi: 10.1037/ccp0000092.
- Garland EL, Hanley AW, Riquino MR, Reese SE, Baker AK, Salas K, Yack BP, Bedford CE, Bryan MA, Atchley RM, Nakamura Y, Froeliger B, Howard MO. Mindfulness-Oriented Recovery Enhancement reduces opioid misuse risk via analgesic and positive psychological mechanisms: a randomized controlled trial. J Consult Clin Psychol. 2019. In press
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-Oriented Recovery Enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. J Consult Clin Psychol. 2014; 82(3): 448-459. Doi: 10.1037/a0035798.
- Garland EL. Restructuring reward processing with mindfulness-oriented recovery enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann N Y Acad Sci. 2016, 1373(1): 25-37. Doi: 10.1111/nyas.13034.
- Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, Skidmore B, Kenny S, Hutton B, Poulin PA. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evid Based Ment Health. 2019; 22(1): 26-35. Doi: 10.1136/ebmental-2018-300062.
- Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016; 315(12): 1240-1249. Doi: 10.1001/jama.2016.2323.
- Garland EL. Disrupting the downward spiral of chronic pain and opioid addiction with mindfulness-oriented recovery enhancement: a review of clinical outcomes and neurocognitive targets. J Pain Palliat Care Pharmacother. 2014; 28(2): 122–129. Doi: 10.3109/15360288.2014.911791.
- Chadi N, McMahon A, Vadnais M, Malboeuf-Hurtubise C, Djemli A, Dobkin PL, Lacroix J, Luu TM, Haley N. Mindfulness-based intervention for female adolescents with chronic pain: a pilot randomized trial. J Can Acad Child Adolesc Psychiatry. 2016; 25(3); 159–168.
- Andrés-Rodríguez L, Borràs X, Feliu-Soler A, Pérez-Aranda A, Rozadilla-Sacanell A, Montero-Marin J, Maes M, Luciano JV. Immune-inflammatory pathways and clinical changes in fibromyalgia patients treated with Mindfulness-Based Stress Reduction (MBSR): a randomized, controlled clinical trial. Brain Behav Immun. 2019. Doi: 10.1016/j.bbi.2019.02.030. In press
- Fjorback LO, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy with older adults: a qualitative review of randomized controlled outcome research. Acta Psychiatr Scand. 2011; 124(2): 102–119. Doi: 10.1111/j.1600-0447.2011.01704.x.
- Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: A randomized controlled pilot study. Pain. 2008; 134(3): 310-319. Doi: 10.1016/j.pain.2007.04.038.