Julia Belinda Poncela-Díaz 1, 2; Melanie Pacheco-Nunes 3, 4; Elena Giménez-Gironda 5, 6; Lucia Gállová 7
1 Faculty of Health Sciences (Nursing), University of La Laguna (ULL)
2 Master´s Degree in ER Critical Care and Emergency Nursing, University of Granada (UGR)
3 Faculty of Philosophy and Letters (Philosophy), University of Granada (UGR)
4 Master’s Degree in Bioethics, Valencian International University (VIU)
5 Faculty of Medicine, University of Valencia (UV)
6 San Cecilio Clinical University Hospital (Granada)
7 Faculty of Health Sciences (Physiotherapy), University of Granada (UGR)
Translated by:
Sabrina Cherif-Aneche 8; Pablo Tocino-López 8; María Campos-García 8; Mercedes Barrera-Bautista 8; Leila Barakat-Ignacio 8
8 Faculty of Translation and Interpreting, University of Granada (UGR)
Introduction
Mechanical restraint (MR) is a fairly common practice despite the controversy surrounding its negative effects and the bioethical dilemmas it raises. The objective of this review is to determine the prevalence and effects of MR in patients, as well as the ethical dilemmas that its use poses for healthcare professionals, while shedding light on prevention and alternative techniques derived from efforts to reduce its use.
Methodology
A systematic search was performed from 2012 to the present in three databases: PubMed, Web of Science and Scopus. Studies related to the health field and to the effects, prevention and alternatives to MR were selected. Excluded studies were: systematic reviews, qualitative studies, studies tested in animals, studies in a language other than English or Spanish, unfinished studies and studies without online full-text access.
Results
Of 115 records found, 20 studies that met the established eligibility criteria were included. The negative effects go from loss of autonomy to risk of pulmonary thromboembolism. The most commonly used methods of prevention and reduction of MR include professional training, multidisciplinary work and individualized treatment plans. The implementation of new strategies based on the use of electronic systems for early identification of risk factors could contribute to prevent MR, although further studies are needed.
Conclusions
Past studies focused mainly on the effects of MR, whereas more recent studies show a clear focus on MR reduction and prevention. The number of new articles on the use of MR is limited due to emerging topics.
Keywords: mechanical restraint, effects, procedures, therapies.
Introduction
The World Health Organization (WHO) defines the mechanical restraint (MR) as extraordinary methods for therapeutic purposes, only acceptable in emergency situations in which there is an urgent or immediate threat to the life or physical integrity of patients or third parties and which cannot be averted by other therapeutic means. MR began to be used approximately 300 years ago; mainly in people who were difficult to control (2) in order to prevent self-harm and physical harm to third parties. Initially, the use of MR was not considered a violation of human rights and was legally approved, so it was widely used in psychiatric hospitals. However, progressive social awareness and greater visibility of the reality of many patients led to discussion of the legal and ethical dilemmas that its use poses (1).
MR can be total if it limits most of the patient’s movements or partial if it limits only the mobility of some limbs or the trunk. MR differs from physical restraint lie in that the latter involves bodily force without using any devices (1,3).
The intention to reduce the use of MR is reflected in laws, principles and amendments related to this practice. One of the problems faced by patients and professionals is the lack of a common legal framework. At the European level, there are references to MR in documents that legislate on human rights such as the Convention for the Protection of Human Rights and Fundamental Freedoms (4). These references are illustrated in practice, where the European Court of Human Rights condemn degrading treatment, opposite to what the Convention says, but it does not condemn physical or mechanical restraints itself (5).
In Spain, Law 41/1986 is directed to those actions that allow the right to healthcare to be effective, without explicitly mentioning MR. Nevertheless, Law 1/1999 of March 31 of Andalusia mentions MR in relation to residential centers, making it necessary for measures depriving users of freedom of movement to be approved by the judicial authority. Moreover, Law 41/2002 established informed consent as essential except in situations where it is necessary to preserve the health and life of the patient (6).
The current indications for the use of MR, according to most protocols, are as follows:
- When there is a risk to the patient’s physical integrity such as falling down or self-harm.
- In the event of physical threat from the patient to third parties.
- In therapeutic settings, as a method to avoid starting medication or catheters, or in situations that require rest and this cannot be achieved in any other way.
MR is associated in some studies with negative effects on both the physical and mental health of patients (7). In addition, it exposes healthcare professionals to some ethical conflicts arising from the confrontation between patients’ rights and their healthcare duties (8-10). For all these reasons, according to recent studies, there has been an increase in the identification of predisposing factors, the study of the effects of MR and the use of alternative methods such as environmental modification or verbal reassurance (6).
Existing protocols are insufficient and should be expanded to reduce the ethical dilemmas arising from the use of MR, supported by a legal framework that responds to these needs (11). For these reasons, together with its clinical relevance, it is important to know the factors that pose a greater or lesser risk of using MR and the alternative methods available. The ambiguity of the current legislation, the heterogeneity of the published research and the actual bioethical dilemmas involved make it necessary to take a highly individualized and a multidisciplinary approach to this topic.
The aim of this systematic review is to determinate the consequences of MR use, both the negative effects on the physical and mental health of patients and the ethical dilemmas that healthcare professionals may face. Other objectives are to delimitate the legal framework of MR and the situations in which it is currently used in specific contexts that is used and to present alternative techniques to replace or prevent the use of MR.
Methodology
After searching three databases (PubMed, Web of Science and Scopus) between February and March, 2021, literature published in the last ten years using the following search equation: “Effects AND Physical Restraint AND Europe”. The results were analyzed by all the authors using PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines (12).The inclusion criteria were: to appear in the selected databases with the search equation used and to deal with MR. The exclusion criteria were: not belonging to the public health field; not dealing with the effects or prevalence of MR or prevention methods and alternatives to its use; to test in animals; being written in a language other than English or Spanish, not having online full-text access, not being qualitative studies; research projects with pending results or systematic reviews.
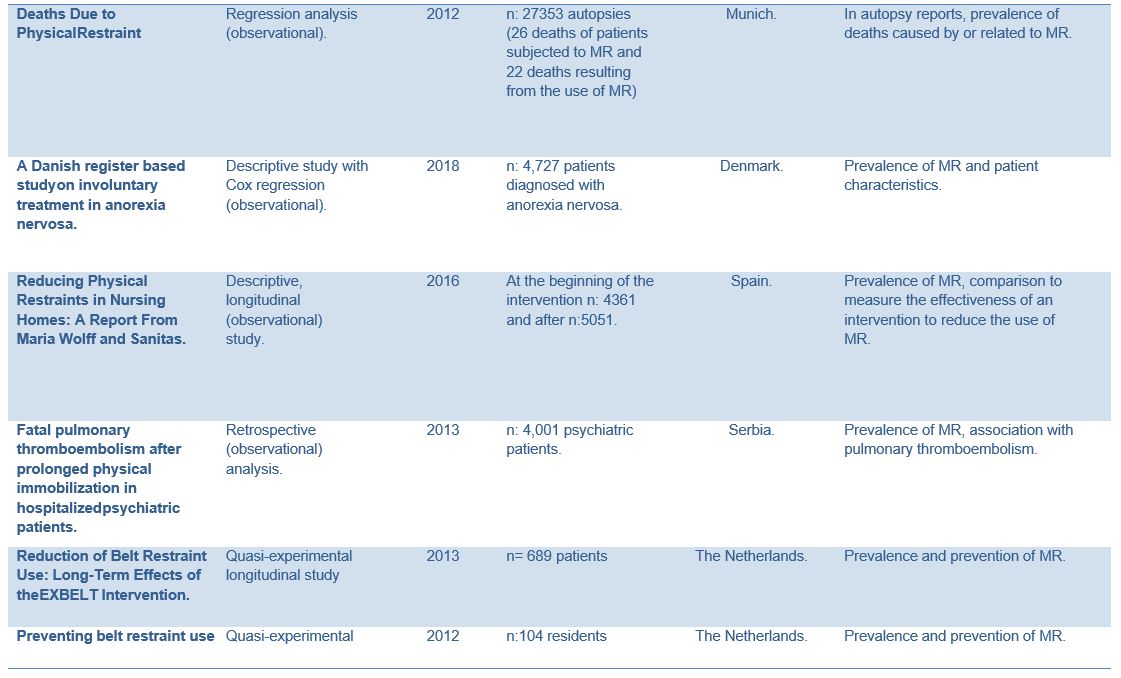
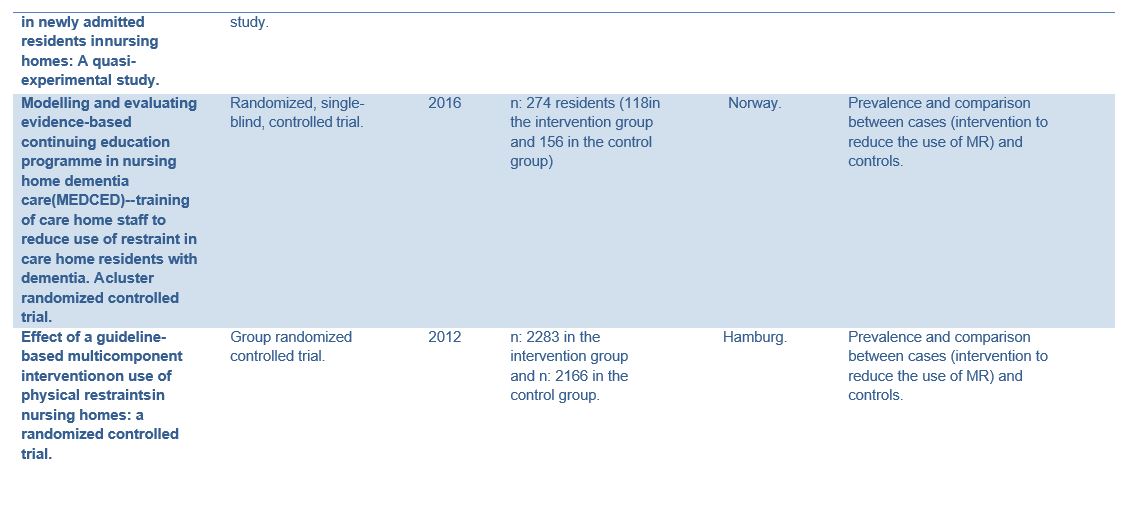
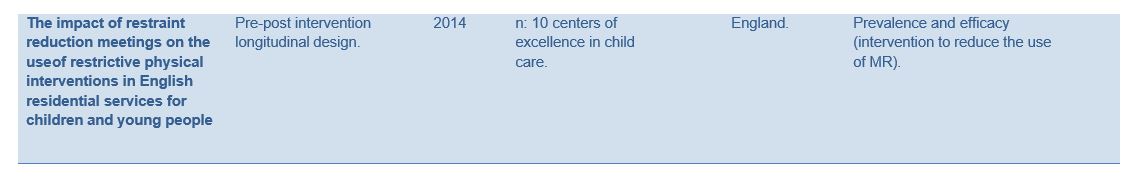
The information was divided into the variables listed in Table 1, subsequently grouping the into three MR areas: prevalence field, effects and alternatives. There is no possibility of bias due to the use of quantitative studies in the results and qualitative studies in the discussion.
Table 1. Variables of interest of the articles included in the results of this systematic review.
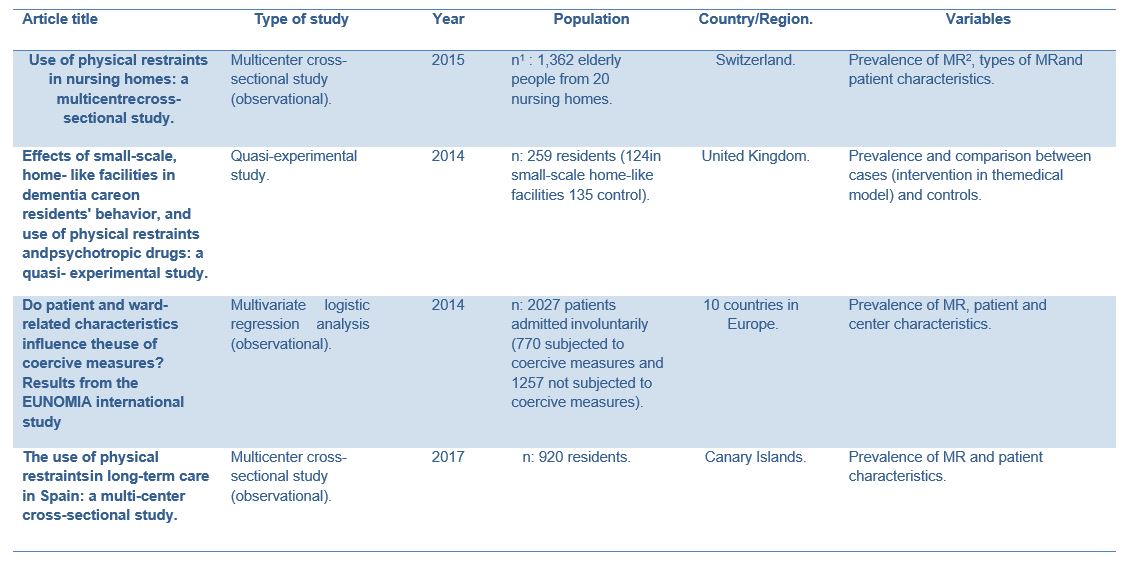
1 N: sample size.
2 CM: Mechanical containment.

Results
Once the search was performed, the studies found up to 8 March, 2021 were included: 112 records in PubMed, 1 record in Web of Science and 5 records in Scopus. The final selection for analysis consisted of 20 studies (Figure 1).
Prevalence of mechanical restraint and effects on patients
MR represents a relevant problem in clinical practice due to its prevalence and effects. Several studies have investigated its negative effects, indicating a growing interest in the development of protocols, programs and therapies to reduce or prevent MR. Research conducted in Switzerland in 2015 on MR in nursing homes found that the prevalence of MR among users was 26.8% and that the most commonly used type of MR was bilateral bedrails (20.3%). Given the high rates of MR, the authors highlighted the need for individualized assessment to use MR and advocated reducing its use (13).
In Denmark, in2018, treatment measures in patients with anorexia nervosa were studied. It was found that, after isolation, the most common measures were physical restraint (51.7%) and mechanical restraint (37.8%) (14).
The prevalence of MR was proved again in another study performed in 2017, in this case in public institutions in the Canary Islands (Spain). The prevalence of residents with at least one form of physical restraint was 84.9%. The main reason for the use of MR was the prevention of falls from beds/chairs (94.2%). In addition, it was determined that people subjected to MR were older and showed a higher level of functional and cognitive impairment and less mobility than those without MR. The degree of impairment was directly related to the probability of suffering restraint. MR was also related to cognitive impairment (15).
Regarding other adverse effects, a 2013 study conducted in Serbia on the effects of the MR suggested a possible association between pulmonary thromboembolisms and the physical immobilization of hospitalized psychiatric patients (16). Another study conducted in Munich in 2012 analyzed patient deaths in relation to MR, showing that 26 deaths in a sample of 2017 users occurred under MR. Additionally, reference was made to other complications such as: in the short term, it was associated with loss of autonomy, freedom and difficulty in social relationships; in the long term, MR caused muscular atrophy or worsened existing atrophy and was also associated with venous thrombosis, stress and negative effects on cognitive abilities. Moreover, incorrect application of the straps led to injuries such as skin abrasions or hematomas. It was also found that, in psychiatry, MR was commonly used to prevent self-harm and suicide attempts. The side rails were the predominant method for care-home residents (17). MR is commonly used in patients with dementia to prevent falls or injuries. Reducing the use MR in these cases may result in increased use of antipsychotic medication, although there are not sufficient studies that can prove this (18).
In 2010 a study was published with data from 10 European countries on psychiatric patients admitted against their will. It showed that patients subjected to MR had higher levels of mistrust, whereas depressive symptoms and anxiety predominated in patients not subjected to it (19).
Prevention and alternatives
Several studies, such as one conducted in Germany in 2012, described the use of interventions to reduce the use of MR and compared the efficiency of these methods. This study indicated that alternative methods to MR can reduce its use from 31.5% to 22.6% (20).
The use of MR and the dilemmas it poses have been highlighted in various studies. Research conducted in 2016 showed that regular use of MR in nursing homes can be an indicator of poor quality of care due to its physical and psychological side-effects. This work focused on reducing the use of MR in nursing homes by introducing a personalized assistance program and educational training of healthcare professionals to safely prevent the use of MR. According to the data, the use of MR was reduced from 18.1% to 1.6%, being even higher in patients with dementia (from 29.1% to 2.2%).
Another study published in 2014, which compared the prevalence of MR in nursing homes in the UK after modifying the patients’ surroundings, showed a significant decrease in its use. (22) Also, a longitudinal study conducted on 10 nursing homes on the use of MR describing the effects of the EXBELT program focused on the use of belts. The program emphasized 4 areas: policy changes regarding MR, an educational program for nurses, inquiries and alternative therapies. Belt use was reduced by 65% in 24 months (23). The same program was investigated in another study on patients with dementia in nursing homes in the Netherlands, proving that EXBELT measures prevented the use of MR in newly admitted patients (24).
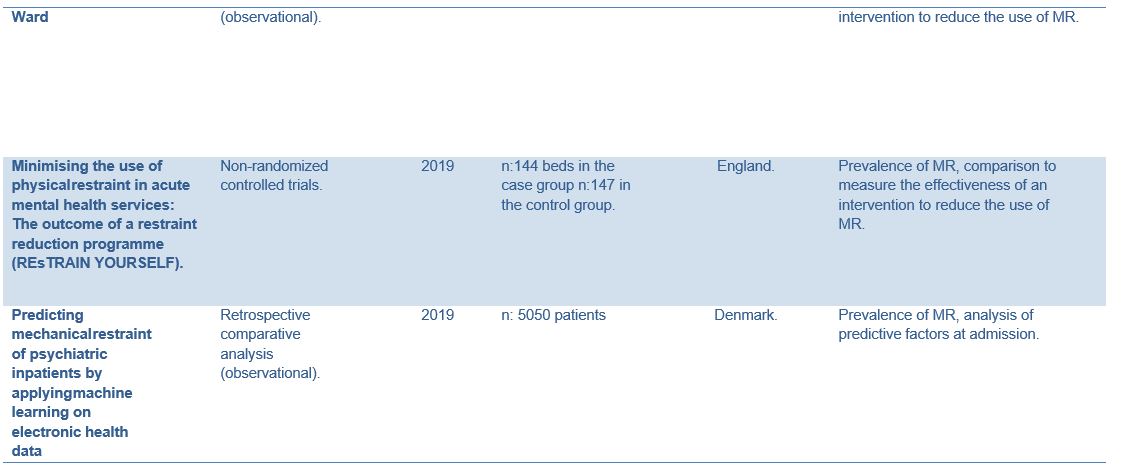
A study was published in 2014, which consisted in the reduction of the frequency and measures of restraint, based on maintaining professional meetings after each MR in English nursing homes for kids and teenagers, with the aim of reducing and preventing future restraints. The study showed a 31.6 decrease of the total use of MR (25).
According to a study conducted in 2014, the most important preventive factor for the reduction of MR was instruction of health workers and nurses, while cognitive milieu therapy and patient-centered care showed to be less productive (26). Nevertheless, a study carried out a year later in psychiatric units in Norway and Denmark showed that there were other factors with a significant effect in the preventing the use MR, such as patient involvement, mandatory review and no crowding. Units that followed individual monitoring of MR cases showed a 64% reduction in prevalence compared with facilities in which monitoring was carried out just in some cases (27).
A study carried out in Spain in 2015 showed that following the implementation of the updated MR protocol at the General Hospital of Málaga, the duration of restraints was significantly decreased, but not its frequency (28). In 2018 a study carried out in southern Germany analyzed the results after the implementation of an intervention to reduce coercive measures. Among these actions were: early identification of patients at risk, an individualized contingency plan on relational and psychopharmacological treatment of patients, the involvement of patients and relatives, incorporation of an occupational therapist to work with sensory integration and a physiotherapist to facilitate physical activity. The use of MR and involuntary medication decreased remarkably in contrast to centers where this intervention was not implemented (29).
The multi-modal approach to MR programs proved to be efficient in prevention, as well as in decreasing the frequency and duration of MR in psychiatric patients. (30) The program REsTRAIN YOURSELF, developed in 2019, decreased MR by an average of 22%. It involved the implementation of Six Core Strategies, a set of alternative techniques to MR. As a result, the ratio of the use MR was significantly lower in intervention rooms (6.62 event/1000 [bed/day]) as compared to control rooms (9.38 event/1000 [bed/day]). Furthermore, previous studies suggested that early identification of patients at high risk for MR could prevent and reduce its use. Risk factors such as schizophrenia, organic mental disorders, being male, living alone and involuntary admission, together with electronic data obtained within the first hours after admission might be identified in order to create an “early warning system” to guide intervention to prevent or reduce MR. (32) The use of machine learning strategies in the identification of patients at risk for MR has the potential to become a powerful tool to prevent MR. Further studies are needed to assess its efficiency.
Discussion
The results of the review showed concern about the effects of MR and the potential alternatives to its use. The dichotomy between benefits and contraindications posed ethical dilemmas for patients and healthcare professionals. Dissatisfaction with its use led its detractors to propose alternative measures, such as the EXBELT practice (23), or the REsTRAIN Yourself initiative (33). However, the use of MR in pain management situations prevailed as the most effective way to treat patients (34). If the main purpose is avoiding or treating pain, what is the most appropriate method?
MR may violate the basic principles of bioethics. Autonomy and justice are compromised when the patient loses the right to self-determination, since MR is usually applied against the patient’s will. Non-maleficence is violated by the effects generated by MR (skin lesions, lung damage, deep vein thrombosis and psychological trauma). MR seeks the beneficence of the patient, even if the rest of the principles are violated (35). Health professionals face dilemmas when MR is used for anything other than preventing self-harm. In addition, factors such as work overload, the clinical condition of the patient, the lack of alternatives to its use, or the lack of protocols for deciding whether it will really benefit the patient also influence the use of MR (34). These factors demand a rapid response, which may lead to excessive use of restraint measures, the balance between risk and safety being ephemeral (36). In addition, subjective factors such as knowing the patient to try to predict her behavior or even to reduce risks to healthcare professionals can significantly influence the use of MR (37).
MR should be used when absolutely necessary, to protect the patient and those around him. It should be the last resort and applied as safely as possible to respect the patient’s dignity. In follow-ups after the use of MR, the ethics and philosophy of care is highlighted to improve care and contribute to prevent immobilization. This is based on recognizing the vulnerability, dependence and dignity of individuals. Without taking this into account, there is no place for assessing patient preferences and needs as an object of study (38).
Currently, there is no evidence to determine the effectiveness of alternatives to MR for all cases, only early assessment and preventive strategies (39). What can be established, however, is that it is frequently put into practice. In Spain, in 2018, 98% of healthcare professionals surveyed used MR of which 82% thought that their training was insufficient. Therefore, many of the negative effects of this practice may stem from a lack of training of healthcare professionals and the absence of protocols on its use (40) (Figure 2).
This systematic review has a number of limitations. More than half of the studies included were observational, which have a lower level of evidence. Also, it was not possible to perform a meta-analysis, since the variables collected were different and those that were not were measured differently among the manuscripts (40).
Conclusion
MR encompasses methods that limit a person’s mobility, partially or totally, using different devices such as straps or belts. In healthcare facilities, it is used to ensure the safety of patients and third parties. The use of MR must be approved and supervised at all times by healthcare professionals. In Europe, its prevalence varies greatly. Studies indicate that its use is not determined by the organizational characteristics of healthcare facilities and that its use in nursing homes is to prevent injuries and falls in patients with dementia, while in psychiatric units it is used in episodes of agitation or violence. Among the negative effects of its use are loss of autonomy and difficulty in social relationships, increased cognitive and functional impairment and an increased risk of thromboembolic events. Finally, restraints imply a lack of freedom for the patient.
Given the negative effects of using MR, there are various interventions to decrease its prevalence in healthcare facilities, nursing homes and psychiatric units. Recommendations include the training of healthcare professionals, the implication of patients and their relatives, the systematic register of all cases in which restraints are used, the use of common rooms instead of individual ones, multidisciplinary work, the use of non-pharmacological soothing methods such as music therapy, or the development of an early assessment of possible episodes of agitation. All these programs have been shown to significantly reduce the use of MR. They emphasize the need for individualization and a multidisciplinary approach to these measures, as they are effective and beneficial for patients.
Statements
Acknowledgements
The authors of this paper would like to thank the involvement of the coordinating and teaching staff of the “Producción y traducción de artículos científicos biomédicos (III ed.)” and the “Traducción inversa de artículos científicos biomédicos (español-inglés)” courses, as well as the English translation team.
Conflicts of interest
The authors of this paper declare no conflicts of interest.
References
- Sastre Rus M, Campaña Castillo F. Contención mecánica: definición conceptual. Rev Ene Enfermería [Internet]. 2014;8:1. Disponible en: https://ene-enfermeria.org
- Masters KJ. Physical restraint: A historical review and current practice. Psychiatr Ann. 2017;47(1):52–5.
- Rubio Domínguez J. Contención mecánica de pacientes. Situación actual y ayuda para profesionales sanitarios. Rev Calid Asist. 2017;32(3):172–7.
- Europeo T, Noviembre DH. Convenio Europeo para la Protección de los Derechos Humanos y de las Libertades Fundamentales revisado de conformidad con el Protocolo n ° 11 completado por los Protocolos n ° 1 y 6. 1998;2:1–16.
- Pichon and Sajous v. Francia. Corte Europea de Derechos Humanos [Internet]. CEJIL, editor. 2011. 145 p. Disponible en: https://www.cejil.org
- López López MT, de Montalvo Jääskeläinen F, Alonso Bedate C, Bellver Capella V, Bellver Capella F, de los Reyes López M, et al. Consideraciones éticas y jurídicas sobre el uso de contenciones mecánicas y farmacológicas en los ámbitos social y sanitario [Internet]. Comité de Bioética de España. 2016. p. 46. Disponible en: https://www.comitedebioetica.es
- Bohorquez de Figueroa A, Carrascal S, Acosta S, Suárez J, Melo A, Pérez J, et al. Evolución del estado mental del paciente sometido a la contención mecánica. Rev cienc Cuid. 2010;7(1):29–34.
- Engberg J, Castle NG, McCaffrey D. Physical restraint initiation in nursing homes and subsequent resident health. Gerontologist. 2008;48(4):442–52.
- Quintero-Uribe LC, Blanco-Arriola L, Zarrabeitia MT. Muertes provocadas por cinturones de contención en ancianos encamados. Rev Esp Med Leg. 2012;38(1):28–31.
- Syamsudin A, Fiddaroini FN, Heru MJA. Minimizing the Use of Restraint in Patients with Mental Disorders at a Mental Hospital: A Systematic Review. J Ners. 2020;14(3):283.
- López J, Ramos P, Gutiérrez J, Rexach L, Artaza I, Moreno N. Documento de consenso sobre Sujeciones Mecánicas y Farmacológicas. [Internet]. Sociedad Española de Geriatría y Gerontología, editor. 2014. 203-218 p. Disponible en: https://www.segg.es
- Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):6.
- Hofmann H, Schorro E, Haastert B, Meyer G. Use of physical restraints in nursing homes: a multicentre cross-sectional study. BMC Geriatr. 2015;15(1):1–8.
- Clausen L, Larsen JT, Bulik CM, Petersen L. A Danish register-based study on involuntary treatment in anorexia nervosa. Int J Eat Disord. 2018;51(11):1213–22.
- Estévez-Guerra GJ, Fariña-López E, Núñez-González E, Gandoy-Crego M, Calvo-Francés F, Capezuti EA. The use of physical restraints in long-term care in Spain: a multi-center cross-sectional study. BMC Geriatr. 2017;17(1):29.
- Stefanović V, Kuzmanović A, Stefanović S. Fatal pulmonary thromboembolism after prolonged physical immobilization in hospitalized psychiatric patients. Vojnosanit Pregl. 2013;70(10):903–7.
- Berzlanovich AM, Schöpfer J, Keil W. Deaths due to physical restraint. Dtsch Arztebl Int. 2012;109(3):27–32.
- Testad I, Mekki TE, Førland O, Øye C, Tveit EM, Jacobsen F, et al. Modeling and evaluating evidence-based continuing education program in nursing home dementia care (MEDCED)–training of care home staff to reduce use of restraint in care home residents with dementia. A cluster randomized controlled trial. Int J Geriatr Psychiatry. 2016;31(1):24–32.
- Kalisova L, Raboch J, Nawka A, Sampogna G, Cihal L, Kallert TW, et al. Do patient and ward-related characteristics influence the use of coercive measures? Results from the EUNOMIA international study. Soc Psychiatry Psychiatr Epidemiol. 2014;49(10):1619–29.
- Köpke S, Mühlhauser I, Gerlach A, Haut A, Haastert B, Möhler R, et al. Effect of a guideline-based multicomponent intervention on use of physical restraints in nursing homes: a randomized controlled trial. JAMA. 2012;307(20):2177–84.
- Muñiz R, Gómez S, Curto D, Hernández R, Marco B, García P, et al. Reducing Physical Restraints in Nursing Homes: A Report From Maria Wolff and Sanitas. J Am Med Dir Assoc. 2016;17(7):633–9.
- Verbeek H, Zwakhalen SMG, van Rossum E, Ambergen T, Kempen GIJM, Hamers JPH. Effects of small-scale, home-like facilities in dementia care on residents’ behavior, and use of physical restraints and psychotropic drugs: a quasi-experimental study. Int psychogeriatrics. 2014;26(4):657–68.
- Gulpers MJM, Bleijlevens MHC, Ambergen T, Capezuti E, van Rossum E, Hamers JPH. Reduction of belt restraint use: long-term effects of the EXBELT intervention. J Am Geriatr Soc. 2013;61(1):107–12.
- Gulpers MJM, Bleijlevens MHC, Capezuti E, van Rossum E, Ambergen T, Hamers JPH. Preventing belt restraint use in newly admitted residents in nursing homes: a quasi-experimental study. Int J Nurs Stud. 2012;49(12):1473–9.
- Deveau R, Leitch S. The impact of restraint reduction meetings on the use of restrictive physical interventions in English residential services for children and young people. Child Care Health Dev. 2015;41(4):587–92.
- Bak J, Zoffmann V, Sestoft DM, Almvik R, Brandt-Christensen M. Mechanical restraint in psychiatry: preventive factors in theory and practice. A Danish-Norwegian association study. Perspect Psychiatr Care. 2014;50(3):155–66.
- Bak J, Zoffmann V, Sestoft DM, Almvik R, Siersma VD, Brandt-Christensen M. Comparing the effect of non-medical mechanical restraint preventive factors between psychiatric units in Denmark and Norway. Nord J Psychiatry. 2015;69(6):433–43.
- Guzman-Parra J, Garcia-Sanchez JA, Pino-Benitez I, Alba-Vallejo M, Mayoral-Cleries F. Effects of a Regulatory Protocol for Mechanical Restraint and Coercion in a Spanish Psychiatric Ward. Perspect Psychiatr Care. 2015;51(4):260–7.
- Højlund M, Høgh L, Bojesen AB, Munk-Jørgensen P, Stenager E. Use of antipsychotics and benzodiazepines in connection to minimising coercion and mechanical restraint in a general psychiatric ward. Int J Soc Psychiatry. 2018;64(3):258–65.
- Guzman-Parra J, Aguilera Serrano C, García-Sánchez JA, Pino-Benítez I, Alba-Vallejo M, Moreno-Küstner B, et al. Effectiveness of a Multimodal Intervention Program for Restraint Prevention in an Acute Spanish Psychiatric Ward. J Am Psychiatr Nurses Assoc. 2016;22(3):233–41.
- Duxbury J, Baker J, Downe S, Jones F, Greenwood P, Thygesen H, et al. Minimising the use of physical restraint in acute mental health services: The outcome of a restraint reduction programme (‘REsTRAIN YOURSELF’). Int J Nurs Stud. 2019;95:40–8.
- Danielsen AA, Fenger MHJ, Østergaard SD, Nielbo KL, Mors O. Predicting mechanical restraint of psychiatric inpatients by applying machine learning on electronic health data. Acta Psychiatr Scand. 2019;140(2):147–57.
- Duxbury J, Thomson G, Scholes A, Jones F, Baker J, Downe S, et al. Staff experiences and understandings of the REsTRAIN Yourself initiative to minimize the use of physical restraint on mental health wards. Int J Ment Health Nurs. 2019;28(4):845–56.
- Sønderskov ML, Hallas P. The use of “brutacaine” in Danish emergency departments. Eur J Emerg Med. 2013 Oct;20(5):370–2.
- Zaami S, Rinaldi R, Bersani G, Marinelli E. Restraints and seclusion in psychiatry: striking a balance between protection and coercion. Critical overview of international regulations and rulings. Riv Psichiatr. 2020;55(1):16–23.
- Cusack P, McAndrew S, Cusack F, Warne T. Restraining good practice: Reviewing evidence of the effects of restraint from the perspective of service users and mental health professionals in the United Kingdom (UK). Int J Law Psychiatry. 2016;46:20–6.
- Perkins E, Prosser H, Riley D, Whittington R. Physical restraint in a therapeutic setting; a necessary evil? Int J Law Psychiatry. 2012;35(1):43–9.
- Hammervold UE, Norvoll R, Vevatne K, Sagvaag H. Post-incident reviews-a gift to the Ward or just another procedure? Care providers’ experiences and considerations regarding post-incident reviews after restraint in mental health services. A qualitative study. BMC Health Serv Res. 2020;20(1):499.
- Fariña-López E, Estévez-Guerra GJ, Polo-Luque ML, Hanzeliková Pogrányivá A, Penelo E. Physical Restraint Use With Elderly Patients: Perceptions of Nurses and Nursing Assistants in Spanish Acute Care Hospitals. Nurs Res. 2018;67(1):55–9.
- Freeman S, Yorke J, Dark P. The management of agitation in adult critical care: Views and opinions from the multi-disciplinary team using a survey approach. Intensive Crit care Nurs. 2019;54:23–8.
AMU 2021. Volumen 3, Número 1
Fecha de envío:
14/03/2021
Fecha de aceptación:
04/04/2021
Fecha de publicación:
31/05/2021