Juan Jesús Pérez-Núñez 1; Pablo Olea-Rodríguez 1; Rafael Manuel Palacios-López 1
1 Faculty of Medicine, University of Granada (UGR)
Translated by:
Celia Martínez-Coronado 2; África Morillas-Steveaux 2; Sergio Ruiz-Martos 2; Mario Sánchez-Cortés-Macías 3; Miguel Sillero Romero 2; Pablo Torregrosa-Parra 4; Diego García-Vergara 5
2 Faculty of Translation and Interpreting, University of Granada (UGR)
3 Faculty of Philosophy and Letters, University of Liège (ULiège)
4 Faculty of Translation and Interpreting, Autonomous University of Barcelona (UAB)
5 Faculty of Humanities, University Pablo de Olavide (UPO)
Introduction
Renal colic (RC) caused by lithiasis is a common reason for presentation to the emergency department. Its diagnosis is usually based on the patient’s clinical picture, but it is sometimes necessary to perform complementary imaging tests. Even though the patient is exposed to high radiation doses, computed tomography (CT) of abdomen and pelvis is the gold standard test to confirm RC by lithiasis. That is why it is necessary to implement and analyze the performance of other imaging tests such as abdominal ultrasound (AUS), which is increasingly becoming more important in clinical practice. The objective of this study was to evaluate the role of AUS in diagnosing a suspected acute RC by lithiasis and the use of other imaging tests in clinical practice.
Methods
This is a retrospective observational study of a cohort of patients with suspected acute RC who underwent an AUS, as requested by the emergency department of a third-level hospital. Different variables related to the patient’s clinical picture, the performed imaging tests and their findings were analyzed. Moreover, both descriptive and analytical analysis of the main variables of interest were conducted: positive diagnosis, use of low radiation dose protocols, and association between pain intensity and other relevant variables.
Results
In this study, a total of 80 patients were analyzed. Of the 64 patients (80% out of the overall sample) who underwent an abdominal radiography (AR), the radiologist was able to detect lithiasis in 18.8% of patients (34.4%), whereas the emergency physician identified it in 7.8% of them (90.6%). The presence of lithiasis was confirmed by AUS in 43.8% of patients. CT was complementarily conducted, diagnosing lithiasis in 38.8% of patients, of whom 90.3% had not been previously diagnosed with lithiasis. A low radiation dose protocol was applied to 48.3% of the latter, and statistically significant differences were found between the mean radiation dose to which those patients were exposed and the one administered when such protocol was not applied. AUS results were neither significantly associated with the pain intensity of the patient’s clinical picture, nor with a previous diagnosis of lithiasis.
Conclusion
AUS is a non-invasive test that offers significant diagnostic results if acute RC is suspected. Low radiation dose protocols are employed in CT with certain frequency when the presence of acute RC is suspected. However, it is necessary to implement intervention protocols that guarantee the appropriate use of this imaging test in clinical practice.
Keywords: urolithiasis, renal colic, ultrasound, computed tomography, emergency department.
Introduction
Renal colic (RC) is an acute pathology characterized by the sudden onset of severe pain in the costovertebral angle. This pain can be located or radiated to the groin (1, 2). The most common cause of this pathology is the obstruction of the ureter by a stone (i.e. urolithiasis). Stones composed of calcium are the most recurrent (3). Lithiasis accounts for 2-5% of all clinical presentations to the emergency department. It is the most common urological emergency (4), affecting 5-10% of the population and presenting a high relapse rate (5).
Sudden pain located in the flanks or radiated to the groin is the most common clinical picture of the patient when treated in the emergency department. This pain can be accompanied by haematuria, urinary syndrome (2) and, less frequently, by gastrointestinal symptoms (nausea and vomiting) or fever, among others (1). To consider it as an acute RC, the patient must present any of the following: fever, renal insufficiency (creatinine >1.5mg/dL), moderate or severe hydronephrosis, bilateral renal colic, solitary kidney, having undergone a renal transplant, uncontrolled pain despite treatment, or pregnancy (1, 6) (Figure 1).
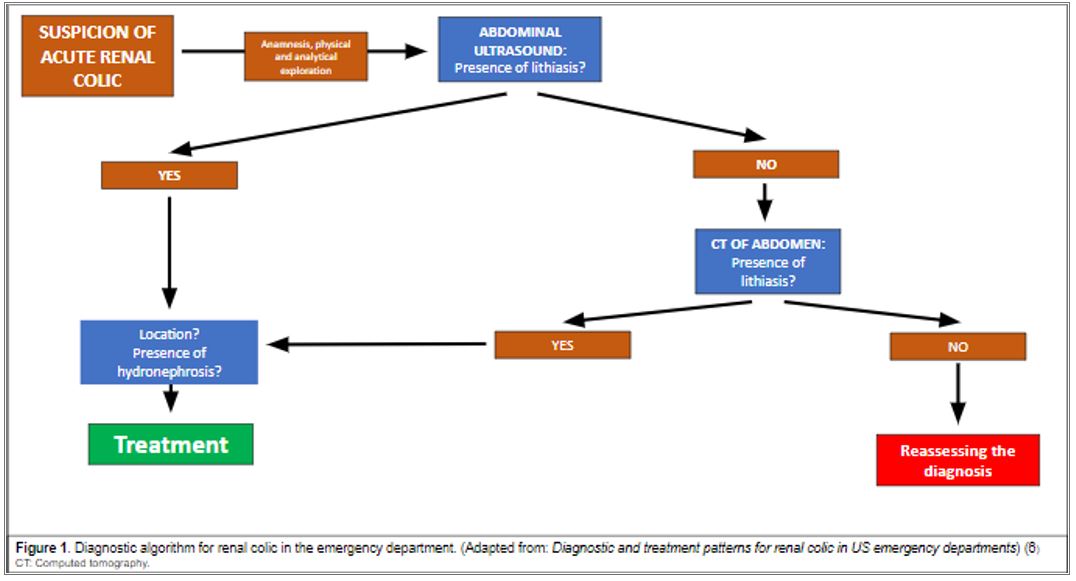
The diagnosis of RC in emergency care is based on three aspects: the patient’s medical record, a urinary sediment analysis, and imaging findings (4). Imaging tests are fundamental to diagnose lithiasis in terms of identifying the location, size and hardness of the stones. Consequently, imaging findings help determine the most appropriate therapeutic options to treat RC. The most common imaging tests performed are plain abdominal radiography (AR), abdominal ultrasound (AUS), and computed tomography (CT) of abdomen and pelvis (7). A urine sediment analysis and an AR are systematically performed on the patient with suspected RC. The results and the development of the patient’s clinical picture will be taken into consideration in order to assess if it is an acute RC or not (4).
CT is considered the gold standard test, as it enables a better examination of the stone than AUS does. Since CT provides more information, the therapeutic decision-making is more appropriate. However, the patient undergoing this procedure is exposed to high radiation doses (13-20 mSv) —unlike AUS— and its routine use is complicated because of the high relapse rate of this illness (2, 6, 7, 10, 11). Therefore, there are low radiation dose protocols to reduce the exposure to 6.1 mSv (11), which is the minimum radiation dose that enables diagnosis by imaging. The effective dose for CT of abdomen and pelvis is around 7.7 mSv (12). AUS solves this problem, but it presents other limitations such as the necessary technical and practical experience of the professional conducting it, the stone size —if it is too small, it may not be visible—, or the patient’s morphotype, among others (13).
Several clinical guidelines recommend AUS as the initial imaging test to be performed on patients with suspected acute RC when AR is anodyne, or the degree of hydronephrosis or other kind of complication must be assessed (7, 10). However, there is a huge variability in the choice and use of imaging tests when RC is suspected in the usual clinical practice (14, 15). Occasionally, ARs are not adequately assessed, or the radiographic technique used is not the most appropriate. Sometimes, the decision of conducting a CT or an AUS is likewise erratic and conditioned by different aspects. On the one hand, the work overload of the on-call radiologist leads to decisions based on aspects such as the patient’s phenotype and the degree of clinical suspicion, among others. On the other hand, when the diagnosis by AUS does not reveal the presence of hydronephrosis, a CT is complementarily performed, but this is not usually conducted in clinical practice. What is more, low radiation dose protocols are neither systematically applied in the performance of this complementary CT (16).
There are few studies that analyze the use and the performance of imaging tests for suspected RC in the usual clinical practice. For this reason, the main objective of this paper is to analyze the role of AUS and other imaging tests in diagnosing suspected acute RC in the usual clinical practice. The secondary objectives of this paper are to describe the clinical and analytical variables of the cohort of patients, and to assess the diagnostic value of the imaging tests that were performed on the patients by the emergency physician and the radiologist. Another secondary objective is to examine associations of potential interest for this research, such as the association between high body mass index (BMI) and the diagnosis of lithiasis by AUS.
Methods
An observational retrospective study was conducted following the STROBE guidelines (17). A retrospective review was made to all the patients who, presenting a suspected acute RC, underwent an AUS from 1st September 2020 to 31st December 2020. This imaging test was requested by the emergency department of Hospital Virgen de las Nieves (Granada, Spain). Pregnant and underage (<18) patients were excluded. This study was approved by the Research Ethics Committee of the Province of Granada (code 1235-N-20).
The database was made in Microsoft Excel®. Laboratory data collected in the emergency department was included: sedimentary red blood cells, creatinine, leukocytes, and C-reactive protein. Data related to the pathology was also included: location and intensity of the pain at the time of requesting the imaging test, assessed by the visual analogue scale (VAS); injured area; presence of vegetative symptoms; and previous diagnosis of RC. In addition, the database contains data from the radiography: the doctor’s or radiologist’s assessment indicating if lithiasis was visible or not, and variables related to AUS performance (presence of vesical filling, visualisation, location and size of the stone, and presence of hydronephrosis). When conducting a CT, the following information was included: use of low radiation dose protocol if applicable and effective dose, as well as the same variables applied to AUS, excluding vesical filling.
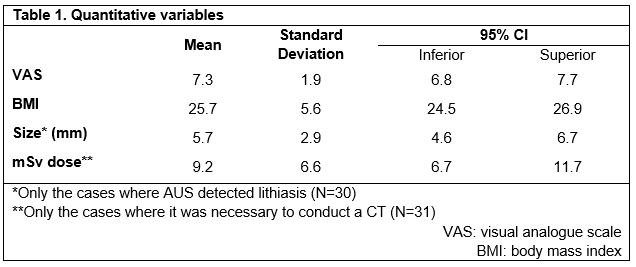
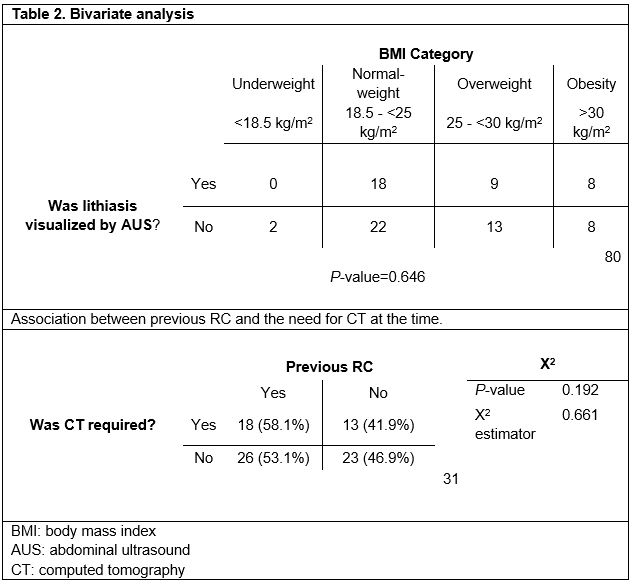
All the variables of the database were statistically analyzed by using SPSS® Statistics 23.0. Furthermore, BMI and its subsequent categorization were calculated: underweight (<18.5kg/m2); normal-weight (18.5 − <25kg/m2); overweight (25 – <30kg/m2) and obesity (>30kg/m2) (18). Some quantitative variables were presented as the median and the standard deviation (Table 1). Two bivariate statistical analyses were undertaken. Firstly, the comparison by Student’s t-test of two means to assess if there were significant differences between the pain assessed by VAS and the detection of lithiasis. Secondly, the χ2 test to analyze the association between a previous diagnosis of RC and the performance of a complementary CT, and between the BMI and the detection of lithiasis by AUS. These data are included in Table 2.
Results
Sample characteristics
The cohort of patients with suspected acute RC, on whom an AUS was performed, was composed of 80 people —49 men (61.3%) and 31 women (38.8%)— with a mean BMI of 25.73kg/m2 (s=5.9; minimum value: 16.4; maximum value: 49.2), and a mean VAS of 7.26 (s=1.95). A CT was performed on 31 patients (38.8%) to confirm the diagnosis of RC, with a mean radiation dose of 9.19 mSv (s=6.57). The low radiation dose protocol was applied to 15 patients (48.3% of the conducted CT). The mean size of the stone detected by AUS was 5.67mm (s=2.87). A descriptive analysis of the following variables was undertaken: BMI, VAS scale, effective dose of mean radiation (mSv) and size of the stone (Table 1). The remaining variables were not taken into account because they were not significant for the objective of this study.
Use of AR
A total of 64 sample patients (80%) underwent AR. An emergency physician examined 90.6% of these radiographies, but lithiasis was only found in 7.8%. Among those analyzed by a radiographer (34.4% of the samples), lithiasis was reported in 18.8%, whereas inconclusive signs were found in 15.6%.
Diagnostic performance of AUS
Obstructive lithiasis was identified by AUS in 35 patients (43.8%). It was located in the distal ureter with a mean size of 4.5 mm (s=2) in 62.9% of the patients; in the middle ureter with a mean size of 7.5 (s=4.5) mm in 5.7%; and in the upper ureter with a mean size of 7.98 mm (s=2.5) in 28.6%. However, 2.9% was not included in the database (lost data).
BMI impact on AUS diagnosis
In our study population, 2 patients (2.5%) were underweight, 40 (50%) were normal-weight, 22 (27.5%) were overweight, and the remaining 16 (20%) were obese. Upon comparison of BMI categories and the presence of lithiasis in the AUS diagnosis, it was found that underweight patients were not diagnosed with lithiasis. Among normal-weight patients, lithiasis was found in 18 out of 40 (45%). In the overweight group, lithiasis was detected in 9 out of 22 (40.9%). As for the obesity group, lithiasis was detected in half of the patients. The χ2 test showed no significant differences among the four groups (p=0.646).
Cases needing CT after AUS
Among our cohort patients, 31 (38.8%) underwent a CT in order to complete the urolithiasis study, which was diagnosed in all the cases. Among these, it was not possible to diagnose it in 28 cases (90.3%) exclusively by AUS. As for the three remaining cases (9.7%), a CT was required to complete the study for other reasons, although it was possible to detect lithiasis by AUS. Among the 45 patients with undiagnosed lithiasis by AUS, 17 (37.8%) did not undergo a CT to complete the diagnosis.
Application of low radiation dose protocol
Within the group that underwent a complementary CT, 15 patients (48.4%) were exposed to a low dose with a mean radiation dose of 5.49 mSv (s=4). The remaining 16 patients (51.6%) were not exposed to this protocol. Among them, radiation data on only 13 patients (81.5%) were collected. These were exposed to a mean radiation dose of 13.46 mSv (s=6.4). The Student’s t-test showed significant differences between the average radiation doses in both groups (p<0.001).
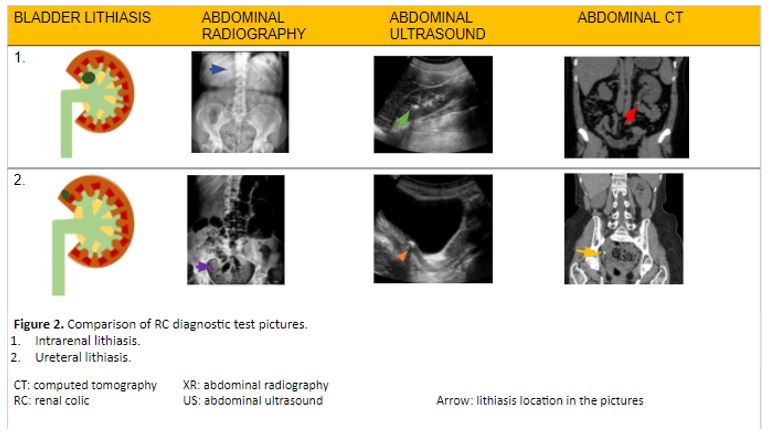
As a summary, Figure 2 shows a comparison between imaging tests (AR, AUS, and CT) in diagnosing RC in the emergency department.
Discussion
Our study presents interesting results. To begin with, the emergency physician identified only 7.8% of urolithiasis cases by a plain AR, whereas 18.8 % of lithiasis cases were identified by the radiographer. The low number of RC cases identified by the emergency physician using AR might be explained by the size of the stone, apart from a poorer training compared to that of the radiographer. According to Sung Li Jung et al. (19), there is an association between a bigger size of the stone and the AR sensitivity (50%) to detect a case of lithiasis. Its sensitivity drops to 23.6% when the stone is smaller than 5 mm. The mean stone size diagnosed by AUS in our study is 5.6 mm. This would explain a decrease in the radiography’s sensitivity to detect urolithiasis. In any case, our results suggest that a cross-consultation with a radiologist should be facilitated so as to aid the diagnosis of renal lithiasis. This would prevent further unnecessary tests, particularly in cases where lithiasis has a small size and is located in the distal ureter.
No significant differences based on the conventional categories of BMI were found in lithiasis diagnosis by AUS, which suggests that this procedure could provide a similar diagnostic performance independently from the patient’s morphotype. However, the reduced sample size of our study requires wider studies, ideally prospective, in order to verify the strength of this hypothesis.
In our study, most urolithiasis diagnosed by AUS have a mean size of 5.67 mm. There are comparative studies that highlight the disadvantage of this procedure regarding the inaccuracy of the urolithiasis diagnosis itself and the size of the stone (13). These studies show that AUS diagnosis tends to overestimate the size of stones smaller than 5 mm. Even Ganesan V et al. (20) point out that there is a significant overestimation in stones up to 10 mm. Such an overestimation can show an increase in the size of stones up to 2.2 mm on average in renal lithiasis. This is not a trivial matter, as clinical management is determined according to the stone size. Therefore, a size overestimation could lead to an inadequate clinical decision for the patient. Some studies reveal that the use of AUS leads to inadequate therapeutic decision-making in 1 out of 5 patients diagnosed by AUS (20).
Smith R et al. (21) observed that patients that underwent AUS are exposed on average to significantly less radiation than those subjected to CT (10.1 mSv and 9.3 mSv, respectively, against 17.2 mSv). However, they confirmed an increase in the need for complementary tests in those patients who underwent AUS at first. The same fact was also observed in our study, as 38.8% of the patients had to undergo a complementary CT after being unsuccessfully diagnosed with RC by AUS. The need for a CT in order to determine with greater accuracy the presence and size of a stone in patients with RC (13) involves exposing patients to radiation (often in several occasions), alongside the dangers it entails for their health, mainly related to radiation-induced cancer (5). As pointed out by Rob S. et al. (22), the frequent use of radiological images in subjects suffering from RC relapses results in exceeding the yearly recommended dose of radiation administered to each patient. Therefore, it supports our idea of encouraging the use of AUS when a case of acute RC is suspected so as to avoid the radiation excess by CT. Low dose (<3.5 mSv) and ultra-low dose (≤1.9 mSv), as defined by Rob et al., correspond to a radiation dose far lower than the mean one used in our study (9.19 mSv). However, if only patients undergoing the low radiation dose protocol are taken into account, the effective doses are similar (mean dose: 5.49 mSv). This aspect is relevant, especially if the fact that the CT diagnostic capacity was not affected is considered. This supports the importance of using these low radiation dose protocols. Nonetheless, it is necessary to verify this matter through specific studies.
It must be noted that there are several limitations in our study. Firstly, the reduced sample size complicates the possibility to establish connections that can be extrapolated to the general population. Secondly, the absence of some potentially interesting variables, such as the reason why CT is performed, why the low dose protocol is administered, and the post-diagnosis type of treatment. Lastly, the study presents a single-center nature that limits the external validity of the study, and there are some lost data due to an inadequate data collection by the healthcare staff. Many of these limitations are due to the eminently practical and descriptive nature of the study. It would be beneficial to establish a common nomenclature in future studies when collecting data on the anatomical site of lithiasis. Among other aspects, this could be used to associate the RC pain intensity with the location of lithiasis.
Conclusions
The RC diagnostic capacity by AUS was acceptable, but the complementary use of CT (the gold standard test) was required in a significant number of cases. According to the scientific literature, the increase in the AUS importance during RC diagnosis is evident, but certain aspects, such as the training of the staff in charge of the test, need some improvements. It is essential to avoid AUS inaccuracies during the diagnosis, as it could lead to a mistaken therapeutic program and an inadequate clinical management of the patient. On the other hand, the plain AR sensitivity is remarkably conditioned by the stone size, as the diagnosis is very limited with small stones. Despite this limitation, the radiographer diagnoses more urolithiasis than the emergency physician, so cross-consultation with the former should be facilitated in order to aid the diagnosis. No associations between a high BMI and a lower ability to visualize urolithiasis in AUS have been found. This would support the use of this technique in patients with a high BMI despite clinical guides advising to perform CT as an initial diagnostic imaging test on this group of patients.
Statements
Acknowledgements
The authors of this paper would like to thank the involvement of the coordinating and teaching staff of the “Producción y traducción de artículos científicos biomédicos (III ed.)” and the “Traducción inversa de artículos científicos biomédicos (español-inglés)” courses, especially Antonio Jesús Láinez Ramos-Bossini for providing us with the radiological images, as well as the English translation team.
Conflicts of interest
The authors of this paper declare no conflicts of interest.
Ethical concerns
This paper has been approved by the Research Research Ethics Committee of the Province of Granada (code 1235-N-20).
References
- Francisco Javier Ancizu FD-C. Cólico renal. [Internet]. [Last access: 29 March 2021]. Available at: https://docplayer.es/111525020-Colico-renal-francisco-javier-ancizu-fernando-diez-caballero.html
- Gary C Curhan, MD S, Mark D Aronson M, Glenn M Preminger M. Diagnóstico y manejo agudo de la sospecha de nefrolitiasis en adultos – UpToDate [Internet]. 2021 [Last access: 5 March 2021].
- Singh P, Enders FT, Vaughan LE, Bergstralh EJ, Knoedler JJ, Krambeck AE, et al. Stone Composition Among First-Time Symptomatic Kidney Stone Formers in the Community. Mayo Clin Proc. 2015; 90(10):1356–65.
- Sánchez-Carreras Aladrén F, Verdú Tartajo F, Herranz Amo F, Escribano Patiño G, María Díez Cordero J, Moncada Iribarren José Jara Rascón I, et al. Urgencias urológicas [Internet]; 2014 [Last access: 8 March 2021]. Available at: https://www.aeu.es/UserFiles/files/Urgencias_Urologicas.pdf
- Aller Rodríguez M, Álvarez Castelo L, Asensi Pernas A, Cabana Cortizas MT, Caeiro Castelao JM, Calvo Quintela L, et al. Abordaje práctico de la patología urológica [Internet]. María Sánchez J, Venancio M, Abal C, editors. EdikaMed, S.L; 2014 [Last access: 8 March 2021]. 277 p. Available at: www.cedro.org
- Brown J. Diagnostic and treatment patterns for renal colic in US emergency departments. Int Urol Nephrol. 2006;38(1):87–92.
- Susaeta R, Benavente D, Marchant F, Gana R. Diagnóstico y manejo de litiasis renales en adultos y niños. Rev Médica Clínica Las Condes. 2018;29(2):197–212.
- Fwu C-W, Eggers PW, Kimmel PL, Kusek JW, Kirkali Z. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013 ;83(3):479–86.
- Coursey CA, Casalino DD, Remer EM, Arellano RS, Bishoff JT, Dighe M, et al. ACR appropriateness criteria® acute onset flank pain-suspicion of stone disease. Vol. 28, Ultrasound Quarterly. 2012.
- Mark L Zeidel M, W Charles O’Neill M. Clinical manifestations and diagnosis of urinary tract obstruction and hydronephrosis – UpToDate [Internet]. 2021 [Last access: 5 March 2021].
- van der Molen AJ, Miclea RL, Geleijns J, Joemai RMS. A Survey of Radiation Doses in CT Urography Before and After Implementation of Iterative Reconstruction. Am J Roentgenol. 2015 [Last access: 29 March 2021];205(3):572–7.
- RadiologyInfo.org | Español [Internet]. [Last access: 29 March 2021]. Available at: https://www.radiologyinfo.org/sp/
- Smith D, Patel U. Ultrasonography vs computed tomography for stone size. BJU Int. 2017 Mar 1 [Last access: 7 March 2021];119(3):361–2. Available at: http://doi.wiley.com/10.1111/bju.13735
- Arrabal Martín M, Barrero Candau R, Campoy Martínez P, Carnero Bueno J, Del Río Urenda S. Urolitiasis: proceso asistencial integrado [Internet]. Junta de A. 2012 [Last access: 12 March 2021]. 230 p. Available at: https://www.juntadeandalucia.es/organismos/saludyfamilias/areas/calidad-investigacion-conocimiento/gestion-conocimiento/paginas/pai-urolitiasis.html
- Robledo Aburto ZA, Borja Aburto VH, Lira Romero JM, Arizmendi Urise E, Peña viveros R. Diagnóstico y tratamiento del cólico renoureteral en el servicio de urgencias. Durango 289-1A Colonia Roma; 2019 [Last access: 29 March 2021].
- Nicolau C, Salvador R, Artigas JM. Diagnostic management of renal colic. Radiología. 2015. 57(2):113–22.
- Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019 (Suppl 1):S31–4.
- F.Xavier P-S, D DMBS, Bouchard C, A R. The Practical Guide Identification, Evaluation, and Treatment of Overweight and Obesity in Adults NHLBI Obesity Education Initiative. 2000 [Last access: 29 March 2021]. 94 p.
- Jung SI, Kim YJ, Park HS, Jeon HJ, Park HK, Paick SH, et al. Sensitivity of digital abdominal radiography for the detection of ureter stones by stone size and location. J Comput Assist Tomogr. 2010;34(6):879–82.
- Semins MJ, Shore AD, Makary MA, Magnuson T, Johns R, Matlaga BR. The Association of Increasing Body Mass Index and Kidney Stone Disease. J Urol. 2010;183(2):571–5.
- Ganesan V, De S, Greene D, Torricelli FCM, Monga M. Accuracy of ultrasonography for renal stone detection and size determination: is it good enough for management decisions? BJU Int. 2017;119(3):464–9.
- Rob S, Bryant T, Wilson I, Somani BK. Ultra-low-dose, low-dose, and standard-dose CT of the kidney, ureters, and bladder: is there a difference? Results from a systematic review of the literature. Vol. 72, Clinical Radiology. W.B. Saunders Ltd; 2017. p. 11–5.
- Smith-Bindman R, Aubin C, Bailitz J, Bengiamin RN, Camargo CA, Corbo J, et al. Ultrasonography versus Computed Tomography for Suspected Nephrolithiasis. N Engl J Med. 2014;371(12):1100–10.
AMU 2021. Volumen 3, Número 1
Fecha de envío:
14/03/2021
Fecha de aceptación:
04/04/2021
Fecha de publicación:
31/05/2021