Violeta De Pablos-Florido 1; Paula María Córdoba-Peláez 2; Paula María Jiménez-Gutiérrez 1
1 Virgen de las Nieves University Hospital (Granada)
2 Faculty of Science (Biochemistry), University of Granada (UGR)
Translated by:
Eva Aguilera-Parejo 4; Rania Bouanane-Hamed 4; Daniel Carmona-Molero 5; Juan Luis Ruiz-García 4; Sheila Vázquez-Ledo 6; David Vilas-Antelo 4
4 Faculty of Translation and Interpreting, University of Granada (UGR)
5 Faculty of Philosophy and Letters, University of Córdoba (UCO)
6 Faculty of Translation, University of Salamanca (USAL)
Introduction
The persistence of COVID-19 sequelae is very common 14 days after acute infection. The term “long-COVID” has been proposed in order to refer to all the secondary conditions to SARS-CoV-2 infection which continue or appear after its acute stage. One of the sequelae is chronic pain with non-demonstrated organ involvement. This systematic review aims to identify the most commonly reported painful sequelae and their incidence.
Methods
A search for articles documenting pain as a consequence of COVID-19 was conducted. The consulted databases were PubMed/Medline, Scopus, and Web of Science. Certain articles cited in the references of relevant articles were also incorporated. Depending on the detailed inclusion or exclusion criteria, three independent researchers carried out the selection. All the articles published before March 11th 2021 were included. This systematic review is based on the PRISMA guidelines.
Results
A total of 588 publications were identified, of which 11 met the inclusion criteria. Headache was the most frequently reported painful sequela, with a prevalence of up to 44% in some cases. Joint pain (19%-31%) and post-COVID thoracic pain (6%-28%) were notified. Persistent sore throat was reported in 32% of patients, as well as generalized pain, observed in up to 59% of the cases. Patient’s polyneuropathy that required admission to the internal care unit (ICU) was additionally notified. SARS-CoV-2 causes damage at the capillary microcirculation level, generating tissue hypoxia and inflammation, with the consequent increase in painful vascular-ischemic and inflammatory sequelae.
Conclusions
COVID-19 produces painful sequelae of various typologies. Subsequent studies are required in order to identify the characteristics of every different type of pain. This will allow an adequate symptomatologic management and an optimization of the available resources to face the challenges of the current pandemic in different healthcare areas.
Keywords: COVID-19, SARS-CoV-2, coronavirus, pain, painful sequelae, long-COVID, post-COVID, persistent COVID.
Introduction
Since the first COVID-19 case reported in Wuhan (1) on December 31st 2019, 116 million people (2) have been infected as of March 21st 2021. Many of them do not fully recover but suffer long-term unspecific chronic pain. These effects are not widely known yet (3). Cases of fatigue, headache, difficulty concentrating, hair loss and dyspnea (3, 12, 18) are reported with high frequency. For this reason, the term “long-COVID” has been suggested in order to bring together all the sequelae that arise two weeks after the disease has passed (4, 8).
It has been demonstrated that presence and severity of somatic symptoms during acute infection are closely related to the subsequent development of chronic fatigue and pain (11, 25). The daily clinical experience of the last few months in the Andalusian Health System (SAS, for its acronym in Spanish, Sistema Andaluz de Salud), has experienced an increase of the influx in healthcare centers of patients with persistent COVID-19 symptoms. These symptoms worsen the quality of life, are difficult to identify in the diagnosis and do not disappear easily with the usual treatments (5). The most common symptoms are myalgia, referred pain, and generalized hyperalgesia (17). They appear in different locations: head (20) and in thorax or limbs (15). Moreover, this disease responds to variable characteristics. Organicity has been ruled out, so the causal mechanism is unknown. However, it is being studied, and it is only associated with convalescence after COVID-19 (8).
It is unknown whether COVID-19 will cause an increase in new-onset chronic pain. The objective of this systematic review is to comprehensively compile reported data on pain as COVID-19 sequela. The secondary objective is to analyze whether the incidence of post-COVID chronic pain during the pandemic has increased. It is of interest to evaluate in future studies the patterns of post-COVID chronic pain, as well as its risk factors, intensity, characteristics, and response to currently used treatment.
Methods
A systematic review of the literature was carried out by three independent researchers (VPF, PCP, and PJG). The consulted databases were PubMed, Scopus and Web of Science. March 11th 2021 was the due date for article selection. In order to increase the sensitivity of the research, the bibliography cited in the articles finally selected was also reviewed. The followed strategy was based on the PRISMA guidelines (24). The search terms were “COVID-19”, “long*”, and “pain”, joined by the Boolean operator “AND”.
Search strategy and selection criteria
Publications available in English or Spanish were identified. Articles analyzing data from patients with pain symptoms more than two weeks after confirmed acute SARS-CoV-2 infection were selected. Non-ambulatory and ambulatory patients which required internal care unit (ICU) admission were included. Only data on the adult population were used. Prospective, retrospective and cross-sectional observational cohort studies were included, as well as systematic reviews and meta-analyses. The titles and abstracts of the articles found in the different databases after applying the search equation were systematically analyzed by independent researchers. Then, the articles which met the inclusion criteria were reviewed completely and jointly by three researchers. Finally, the inclusion or exclusion of the studies was discussed.
Inclusion and exclusion criteria
Publications in languages other than English or Spanish, and whose study population included children (under 18 years of age) and pregnant women were excluded. Any symptomatology secondary to COVID-19 after at least two weeks following the acute stage was considered to be a persistent sequela. Studies with a sample size of less than 50 individuals were rejected.
Data extraction of the included articles
The references found on the systematic research were imported into the Zotero reference manager. After removing duplicate items, a single reference folder was created. The following information was chosen from the selected articles: number of subjects studied, country where data were collected, mean age, sex, healthcare setting (inpatient, outpatient, ICUs, healthcare staff) and mean follow-up time. The main objective of each study was pointed out, as well as the enumeration of the sequelae observed. Symptomatology related exclusively to pain was also extracted. The prevalence of pain in different locations of the body was expressed in percentages, and their characteristics were listed.
Results
A total of 678 articles, retrieved as a result of the defined search equation, were reviewed based on their title and abstract. Subsequently, 54 publications were selected by independent researchers, who fully read all of them. Of them, 43 were excluded due to not meeting the inclusion criteria. The specific reasons for exclusion were the following: 12 articles addressed chronic symptoms but did not include pain; 14 were single case reports or had sample sizes of less than 50; 4 were letters to the editor; 9 focused on acute or non-painful symptoms; 2 did not meet age criteria; 1 did not meet language criteria; and 1 studied non-COVID population. A total of 11 studies were finally selected for analysis.
Most of the studies identified were published between July 2020 and January 2021: 4 were transversal studies; 5 were cohort studies; 3 were retrospective; 2 were prospective; and 1 was a systematic review. The systematic review involved multi-center studies. In the case of the other studies, 4 were carried out in the USA (one of them included 13 North American states); the remaining ones in Italy, Spain, Switzerland, France, and Egypt.
Most of the studies were carried out by means of surveys of patients recovered from acute SARS-CoV-2 infection, on an outpatient basis and sometimes by phone due to the restrictions of home confinement during the pandemic. Of those publications, 5 focused on patients that required hospitalization, 2 on outpatients that experienced the acute phase of the disease, and 4 are not known to have required hospitalization. An average of 697 patients were included in the selected studies. The mean age of the subjects was 45 years, with no differences regarding the sex of the patients studied.
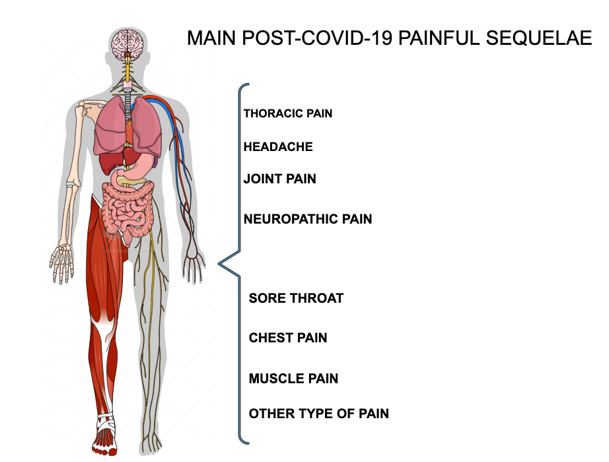
Of all the included studies, headache is the most frequently reported painful sequela, with a reported prevalence of up to 44% after acute infection according to Sandra López-León et al. (4). Two articles reported results on muscle pain (4, 18). Joint pain as a sequela after two weeks of infection was reported at 19% and 31% (4, 23). Post-COVID-19 thoracic pain was reported in a percentage range of 6% to 28% of patients included in the studies (20, 23, 24, 25). Persistent sore throat was reported in 32% of patients, and non-specific or generalized pain was observed in up to 59% of cases, according to the study by Tenforde et al. (25). Neuropathic pain secondary to polyneuropathy in critically ill patients was significant among patients that required a prolonged ICU admission (15, 17). Figure 1 shows a visual scheme of the different painful sequelae.
Figure 1. Most common post-COVID-19 painful sequelae
In addition, SARS-CoV-2 has been reported to cause damage to at the capillary microcirculation level, leading to tissue hypoxia and inflammation, and consequently to an increase in painful vascular-ischemic sequelae (6). It has also been reported that high levels of persistent antibodies after the infection are associated with fever, diarrhea and other sequelae (7).
Discussion
The COVID-19 pandemic is a revolution for healthcare as we know it. Firstly, because of the change it has caused in clinical care. Secondly, because of the pathophysiology of the disease, which remains largely unknown. Lastly, because of how it is affecting and will affect people’s health (8).
The COVID-19 pandemic has led many health services to cease or reduce their activity. Treatments have been delayed or stopped (9, 10), resulting in negative effects such as increases in patients’ chronic pain, disability and depression (13, 14, 39). The emergence of telemedicine as a barrier tool to curb the spread of the virus makes more necessary than ever engaging patients in their own health. Healthcare professionals must pay close attention to properly educating patients on their underlying pathology and pain management options, while involving them in participatory decision-making processes. Telemedicine appears to be a promising resource in the management, treatment and follow-up of patients with chronic pain (10, 17, 39).
In addition, the painful sequelae of COVID-19 seem to respond to different etiopathogenic mechanisms. Reports range from headache, in mild forms of the disease, to painful inflammatory neuropathies in critically ill patients (32). Muscle pain is common in both mild and severe forms (33). The spectrum of ischemic pain has also emerged as a complication, linked to hypercoagulability and associated microcirculatory dysfunction (7). All of this is currently being researched in order to achieve a better understanding of the disease and the long-term symptoms it may cause.
Meanwhile, the contagiousness period for patients with a positive SARS-CoV-2 screening test is approximately twenty days (40). Once recovered from the acute symptoms, they are discharged from the hospital services where they have been treated (21). Many centers have already set up multidisciplinary units to follow up discharged patients after admission for COVID-19. However, there is also a large number of patients with post-COVID-19 pain who suffered a mild or moderate paucisymptomatic acute infection, who are left out of these units because they were treated and followed up on an outpatient basis (4, 22, 25, 26, 27). Emphasis is placed on the quality of healthcare for those who, while “recovered” from the acute infection and out of danger, still suffer from symptoms that limit their quality of life (28). This study tried to shed light and prove that post-COVID-19 chronic pain is a reality which is sometimes underestimated and undertreated. For that reason, the results of this analysis, supported by other studies, suggest the importance of setting up multidisciplinary units to care for the patients whose original condition was less severe. It is crucial that they receive long-term medical follow-up, aimed at detecting and treating symptoms derived from SARS-CoV-2 infection (3, 4, 5, 11, 25, 36).
It is of great interest to evaluate in future studies the approach to post-COVID-19 pain according to location, characteristics and response to the treatments carried out.
Limitations
The selection of articles by independent reviewers constituted a limitation, in terms of accuracy, during the literature research. This was expanded with literature taken from the references of the articles selected. The large databases consulted provided articles with little relation to COVID-19, in contrast to the new large library LitCovid, a database focused exclusively on SARS-CoV-2 (22). In addition, most of the selected articles did not address pain as the only sequela of COVID-19. There is still a lack of studies that provide larger sample sizes, as well as prospective studies that address pain sequelae in their temporal dimension. The characteristics, intensity, localization and other variables need to be examined in more depth to better classify pain as a sequela of COVID-19.
Conclusions
For many patients, COVID-19 infection does not end after acute infection recovery. At present, long-COVID phenomena are not well understood, let alone their potential consequences. Several lines of research aimed at shedding light on the natural history of a disease that is being experienced in real time. COVID-19 has painful sequelae of various typologies. There is already evidence of an increase in the incidence of post-COVID-19 chronic pain. Further studies are required to identify the characteristics of the different types of pain. The need to make appropriate use of telemedicine is emphasized. Moreover, multidisciplinary units that receive and study long-COVID cases are needed. This will allow a proper symptomatologic management and an optimization of the available resources to face the challenges of the current pandemic in different healthcare areas.
Statements
Acknowledgements
The authors of this paper would like to thank the involvement of the coordinating and teaching staff of the “Producción y traducción de artículos científicos biomédicos (III ed.)” and the “Traducción inversa de artículos científicos biomédicos (español-inglés)” courses, especially Antonio Jesús Láinez Ramos-Bossini for his support and mentorship, as well as the English translation team.
Conflicts of interest
The authors of this paper declare no conflicts of interest.
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf Dis. 20(5):533-534. doi: 10.1016/S1473-3099(20)30120-1.
- Carfì A, Bernabei R, Landi F, Gemelli. Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324(6):603-5.
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. MedRxiv Prepr Serv Health Sci. 2021.
- Gemelli Against COVID-19 Post-Acute Care Study Group. Post-COVID-19 global health strategies: the need for an interdisciplinary approach. Aging Clin Exp Res; 32(8):1613-20.
- Amjadi MF, O’Connell SE, Armbrust T, Mergaert AM, Narpala SR, Halfmann PJ, et al. Fever, Diarrhea, and Severe Disease Correlate with High Persistent Antibody Levels against SARS-CoV-2. medRxiv. ;2021.01.05.21249240.
- Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiological Reports. 2021; 9(3):e14726.
- Walitt B, Bartrum E. A clinical primer for the expected and potential post-COVID-19 syndromes. PR9. 2021; 6(1):e887.
- Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, Bhatia A, et al. Caring for patients with pain during the COVID ‐19 pandemic: consensus recommendations from an international expert panel. Anaesthesia. 2020; 75(7):935–44.
- Lynch ME, Williamson OD, Banfield JC. COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics. Canadian Journal of Pain. 2020; 4(1):204–9.
- Vittori A, Lerman J, Cascella M, Gomez-Morad AD, Marchetti G, Marinangeli F, et al. COVID-19 Pandemic Acute Respiratory Distress Syndrome Survivors: Pain After the Storm? Anesthesia & Analgesia. 2020;131(1):117–9.
- Willi S, Lüthold R, Hunt A, Hänggi NV, Sejdiu D, Scaff C, et al. COVID-19 sequelae in adults aged less than 50 years: A systematic review. Travel Medicine and Infectious Disease. 2021; 40:101995.
- Hruschak V, Flowers KM, Azizoddin DR, Jamison RN, Edwards RR, Schreiber KL. Cross-sectional study of psychosocial and pain-related variables among patients with chronic pain during a time of social distancing imposed by the coronavirus disease 2019 pandemic. Pain. 2021;162(2):619–29.
- Louw A. Letter to the editor: chronic pain tidal wave after COVID-19: are you ready? Physiotherapy Theory and Practice. 2020; 36(12):1275–8.
- Orsucci D, Caldarazzo Ienco E, Nocita G, Napolitano A, Vista M. Neurological features of COVID-19 and their treatment: a review. DIC. 2020;9:1–12.
- Little P. Non-steroidal anti-inflammatory drugs and covid-19. BMJ. 2020; m1185.
- El-Tallawy SN, Nalamasu R, Pergolizzi JV, Gharibo C. Pain Management During the COVID-19 Pandemic. Pain Ther. 2020;9(2):453–66.
- Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. Madeddu G, editor. PLoS ONE. 2020;15(12):e0243882.
- Porta‐Etessam J, Matías‐Guiu JA, González‐García N, Gómez Iglesias P, Santos‐Bueso E, Arriola‐Villalobos P, et al. Spectrum of Headaches Associated With SARS‐CoV‐2 Infection: Study of Healthcare Professionals. Headache: The Journal of Head and Face Pain. 2020;60(8):1697–704.
- Somani SS, Richter F, Fuster V, De Freitas JK, Naik N, Sigel K, et al. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization for COVID-19. J Gen Intern Med. 2020;35(10):2838-44.
- Nehme M, Braillard O, Alcoba G, Aebischer Perone S, Courvoisier D, Chappuis F, et al. COVID-19 Symptoms: Longitudinal Evolution and Persistence in Outpatient Settings. Ann Intern Med. 2020.
- PRISMA. Available at: http://prisma-statement.org/prismastatement/flowdiagram
- Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post-COVID-19 manifestations. Int J Clin Pract. 2020;e13746.
- Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81(6):e4-6.
- Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network – United States, 2020. MMWR Morb Mortal Wkly Rep. 31 de julio de 2020;69(30):993-8.
- Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, et al. Autonomic dysfunction in «long COVID»: rationale, physiology and management strategies. Clin Med (Lond). 2021;21(1):e63-7.
- Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20.
- Nagu P, Parashar A, Behl T, Mehta V. CNS implications of COVID-19: a comprehensive review. Rev Neurosci. 2021;32(2):219-34.
- Abboud H, Abboud FZ, Kharbouch H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 Infection: Pathophysiology and Clinical Effects on the Nervous System. World Neurosurg. 2020;140:49-53.
- Berger JR. COVID-19 and the nervous system. J Neurovirol. 2020;26(2):143-8.
- Neufeld KJ, Leoutsakos J-MS, Yan H, Lin S, Zabinski JS, Dinglas VD, et al. Fatigue Symptoms During the First Year Following ARDS. Chest. 2020;158(3):999-1007.
- Membrilla JA, de Lorenzo Í, Sastre M, Díaz de Terán J. Headache as a Cardinal Symptom of Coronavirus Disease 2019: A Cross-Sectional Study. Headache. 2020;60(10):2176-91.
- Sher L. Post-COVID syndrome and suicide risk. QJM. 2021.
- Barker-Davies RM, O’Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949-59.
- Chen Q, Allot A, Lu Z. LitCovid: an open database of COVID-19 literature. Nucleic Acids Research. 2020.
- Vidal-Alaball J, Acosta-Roja R, Pastor Hernández N, Sanchez Luque U, Morrison D, Narejos Pérez S, et al. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria. 2020;52(6):418-22.
- Xiao AT, Tong YX, Gao C, Zhu L, Zhang YJ, Zhang S. Dynamic profile of RT-PCR findings from 301 COVID-19 patients in Wuhan, China: A descriptive study. J Clin Virol. 2020;127:104346.
AMU 2021. Volumen 3, Número 1
Fecha de envío:
14/03/2021
Fecha de aceptación:
04/04/2021
Fecha de publicación:
31/05/2021